HIV - None of Our Business
I remember wondering if I could catch HIV off a toilet seat when sharing a holiday house with a friend living with HIV in 2009. That’s where my knowledge around HIV was back then. Those tombstone adverts from the 80’s stuck in our minds, this was a death sentence, and anyone could catch it.
That couldn’t be less true, and I want to help educate our industry to get up to date on the facts, the law and why you shouldn’t have the question on your consultation forms.
Let’s debunk the myths surrounding HIV and beauty treatments, so no one ever feels discriminated against, so no one living with HIV ever feels shame or embarrassment.
There are many misconceptions surrounding HIV and beauty treatments, especially in relation to services such as electrolysis and semi-permanent make-up, whether status disclosure is necessary, how medication interacts and if healing is slower in someone living with HIV.
These are all valid questions, but not ones your clients need to answer.

Let’s start with what is HIV?
HIV stands for human immunodeficiency virus, a virus which weakens the human immune system. The immune system is our natural defence that protects us against disease and ill health.
If left undiagnosed and untreated HIV can cause damage to the immune system which can leave people vulnerable to other infections.
HIV is a long-term health condition that is easily manageable with medication which effectively reduces the amount of the virus in the body to the point where it cannot be detected. HIV treatment has made huge advances, with 97% of people living with HIV in the UK on treatment. The life expectancy of someone living with HIV is now the same as it would be for someone without the conditions. Public perceptions, and societal knowledge about HIV have not kept pace with medical advancements and improved prognosis.
What does U = U mean?
Fear around HIV transmission can fuel HIV stigma, and that the U=U message is one of the most powerful ways in which HIV stigma will be defeated.
‘U = U’ means ‘undetectable = untransmissible’. Undetectable simply means that a person living with HIV’s viral load (the level of HIV in their blood) is so low that it can’t be detected by tests it also means that HIV cannot be transmitted through sex. We know this because of rigorous scientific studies and research.
For most people, this takes between four weeks and six months. A patient is officially classed as undetectable after two undetectable blood tests, and they are usually tested after four weeks, eight weeks and then three months after starting medication. Then they continue to get tested every six months.
Whilst fully endorsing the U=U message and ensuring ongoing support for people to have and sustain an undetectable viral load, it is vitally important that people who, for whatever reason, do not, or cannot, achieve an undetectable viral load are not seen, or treated, any differently than people who do.
What is the law around HIV disclosure?
People living with HIV are not legally obliged to tell anyone about their status – whether that’s a sexual partner, medical professional, or beauty therapist. They don’t even have to tell their doctor or dentist (although it is encouraged).
Most people living with HIV are afraid to be open about their status because of fear of stigma, so a situation, like the tick-box exercise on a consultation form, could be really damaging to their mental health.
Do I need to have HIV on my consultation form?
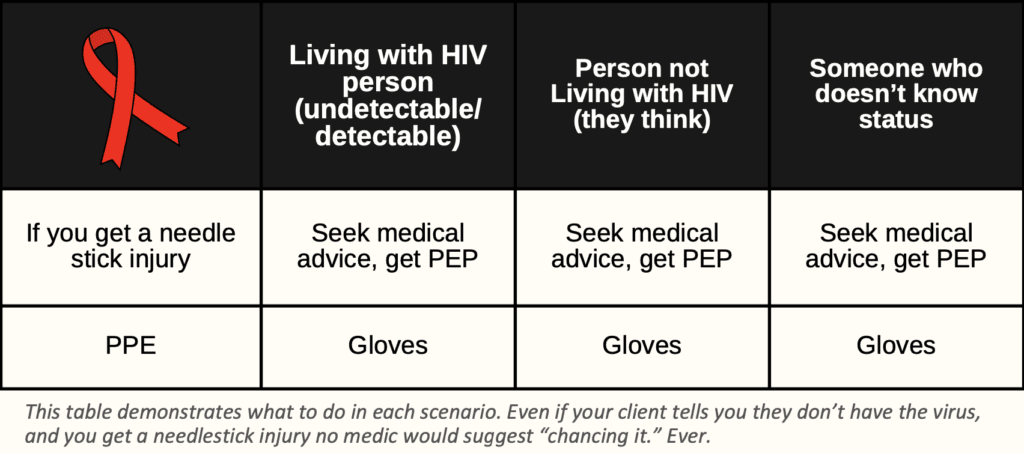
There has never been a recorded HIV transmission from piercings, tattoos, or any other cosmetic beauty treatment. It is incredibly hard to contract HIV in general. It loves that warm body environment, so with things like needlestick injuries or blood splatters, it is almost impossible to contract it. It takes less than a minute for HIV to die outside the human body in a blood spill.
I spoke to standards-setting body Habia and they confirmed that the rules you should be following [for clients living with HIV] are our universal hygiene procedures.
If you ask about HIV on your consultation form, ask yourself these questions:
Why do you need to know it?
What will you do with that information?
How are you going to treat that person differently?
Are you basing your hygiene protocols on asking someone if they have a contagious blood disorder?
Think about these questions because if it doesn’t affect your practice then it doesn’t need to be on your form. Plus, of those who know they have HIV, 97% are on treatment and are virally supressed, so there is no risk. Most transmissions occur when people aren’t aware of their status and have a higher viral load, but even then, that would not be a risk factor in a beauty setting when following universal precautions.
Can I refuse to treat a client living with HIV?
There is a joint statement from the British HIV Association, British Association of Sexual Health and HIV, National Aids Trust, Terrence Higgins Trust, and HIV Scotland regarding reports of discrimination against people with HIV from some providers of cosmetic treatments and tattooing.
“Refusing to tattoo or to provide a cosmetic or routine beauty treatment to a client based on their HIV status cannot be justified. To do so would constitute discrimination under the Equality Act 2010. The Equality Act 2010 prohibits discrimination against a range of protected characteristics.
“In the Act, any person with HIV is protected under the category of disability. Collecting information about HIV status must be justifiable, as per current data protection legislation (Data Protection Act 2018 and General Data Protection Regulation 2018), and is unnecessary in the context of tattooing, piercing, and cosmetic or routine beauty treatments.
“HIV and HIV treatment are not contraindications to tattooing, piercing or cosmetic procedures, so it is not necessary to collect information on HIV when assessing clients prior to these.”
You can refuse treatment because that person is unwell, or they have another contraindication, but you need a valid reason to refuse treatment for any client, and HIV is never the reason.
What language should I/shouldn’t I use when engaging with a client living with HIV?
Language is everything here – some of the words used about HIV, and people living with HIV, can have stigmatising connotations, the main one is to avoid using “HIV-positive person” or “person who has HIV” as it’s better to use “person living with HIV” because it puts the person before the diagnosis. Having HIV does not define the person. Also avoid using negative terms like ‘victim’ or ‘sufferer.’
See George House Trust’s HIV Language Guide below.
Do people have AIDS?
Another common misconception is that AIDS can be passed on. This is not the case. HIV, the virus which can lead to AIDS (Advanced HIV), can be passed between individuals, but AIDS is merely a term used to describe a collection of illnesses.
AIDS stands for acquired immune deficiency syndrome and is not the same as HIV. It is unlikely that the term AIDS would be used these days, particularly in healthcare. Advanced or late-stage HIV is how this would be referred to. Even if someone becomes extremely ill with HIV, as long as it is diagnosed and treated in time for the immune system to recover, then the person can recover to some extent. Early diagnosis and treatment are the key to avoid this happening.
No one “has AIDS,” you cannot catch AIDS and there is no such thing as an AIDS test.
What if I want to know about existing conditions/medications to ensure the client won’t have an adverse treatment reaction?
We need to take a full medical history for certain treatments, but asking someone’s HIV status bears no relevance. HIV medication does not interact with any beauty treatments. What I ask all my clients for advanced treatments is “How do you heal?” This is inclusive and can be asked to everyone.
Don’t people living with HIV heal differently?
One of the most common misconceptions is that those living with HIV cannot have certain treatments as they heal slower than those who aren’t living with HIV.
Dr Stephen Higgins, consultant physician in the department of sexual health and HIV at North Manchester General Hospital, confirmed “People living with HIV heal the same way as anyone else, so there’s no reason at all to refuse someone (cosmetic) treatment because of their medication.”
Paul Fairweather, who works for George House Trust also commented “My count for how strong my immune system was 900 last time, which is well within the usual range. My health is fine, my life expectancy is normal, and, in fact, there’s been research showing that people living with HIV have a higher life expectancy than those who don’t because we have so many check-ups and get our health monitored.”.
In 2024 George House Trust and I will be bringing out a free guide with specifically for the hair, beauty and barbering industry. Register your interest here HIV Beauty Campaign | George House Trust (ght.org.uk)
Sam Marshall
To connect with Sam you can visit her listing here

